Medicaid members face losing continuous coverage as states prep for end of COVID-19 public health emergency

The COVID-19 public health emergency required states to continuously cover Medicaid program members until the emergency officially ends. In exchange for enhanced federal funding, states were barred from disenrolling people from the programs. (WABE)
The state is preparing for the anticipated end to the federal government’s COVID-19 public health emergency that’s extended Medicaid programs during the pandemic. This means Georgia Medicaid and PeachCare for Kids members are required to update their contact information in the system and prepare to recertify.
Under the COVID-19 public health emergency, states have been required to continuously cover Medicaid program members until the emergency officially ends. In exchange for enhanced federal funding, they were barred from disenrolling people from the programs.
The provision was designed to make sure people had uninterrupted health coverage during the coronavirus crisis.
Around 2.6 million Georgians currently rely on Medicaid or PeachCare for Kids.
For many people who were continuously covered during the pandemic, this will be their first time going through the regular redetermination process.
Health advocates have expressed concern that the so-called Medicaid unwinding process could open eligible people up to erroneously losing their insurance coverage.
The federal public health emergency is expected to remain in effect until at least mid-January.
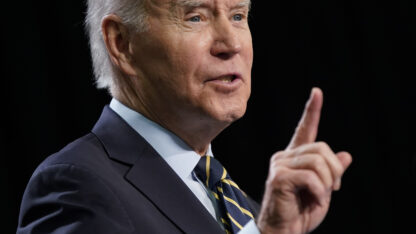
Whenever the Biden administration discontinues it, all states will be required to review their Medicaid program members’ eligibility within just over a year.
In preparation, officials with the Georgia Department of Human Services and the Georgia Department of Community Health are asking members to verify their contact information.
To update your information, go to gateway.ga.gov calling (877) GA-DHS-GO, or visiting your local DFCS office.