More than six months into 'unwinding,' Georgia sees high numbers of children losing Medicaid

Health advocates in Georgia are expressing concern over the state’s handling of the Medicaid redetermination process after a Biden administration report found Georgia is among the states with the highest percentages of children unnecessarily losing their coverage.
During the first six months of unwinding its Medicaid pandemic protections, Georgia cut off health insurance coverage for more than 149,000 children, many of whom remain qualified for the safety net program.
The data demands urgent attention, said Georgia Budget and Policy Institute Director of Health Justice Leah Chan.
“Ensuring access to comprehensive health coverage is not just a policy goal; it is a fundamental commitment to the well-being of our children and the financial security of hardworking families. No child should lose their health coverage due to bureaucratic hurdles or avoidable reasons,” she said, “especially as we transition from the continuous enrollment provision established during the COVID-19 public health emergency.”
Until late spring of 2023, federal COVID-19 pandemic rules had barred states from removing anyone from their Medicaid rolls. With the prohibition lifted, states are mandated to reevaluate eligibility for all adults and children with Medicaid coverage.
In Georgia, that means roughly 2.8 million adults and children must now submit applications to renew their coverage.
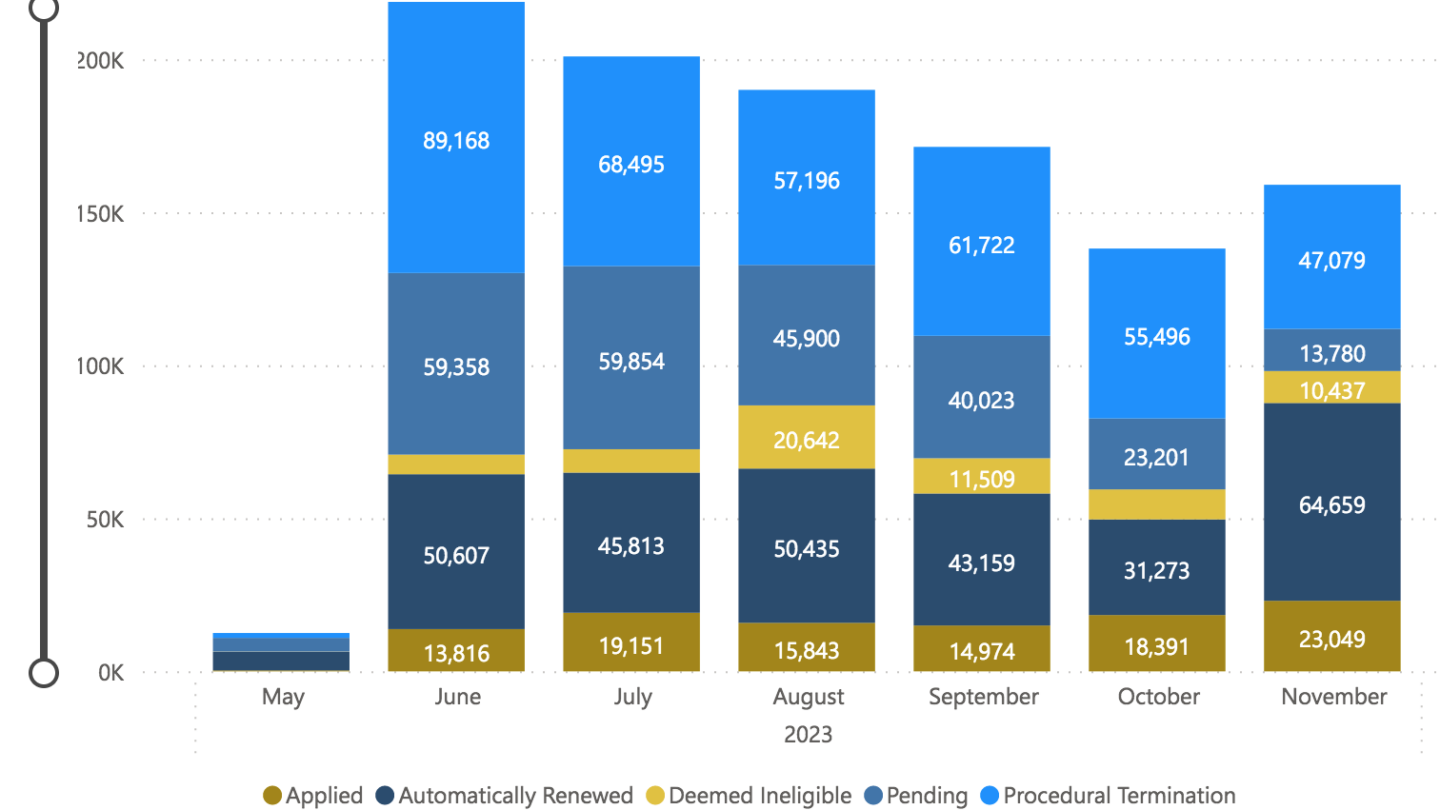
And, as of November, the state has processed just under 1.1 million Medicaid renewal applications.
Of those, 380,737 people have so far lost their health insurance for “procedural” reasons, which include paperwork or mail problems, or missed deadlines — red tape.
U.S. Department of Health and Human Services (HHS) Sec. Xavier Becerra sent a letter to each of the nine states with the highest child Medicaid terminations, including Georgia.
“We’re calling on removing barriers that make it difficult for families to transition to CHIP coverage if they are no longer eligible for Medicaid coverage. We call on reducing call center wait times and partnering with pediatric providers, managed-care plans, schools and community organizations to reach additional families in need. And we call on expanding their Medicaid programs if they have not done so already to ensure everyone has access to affordable coverage options that qualify that they don’t fall into the coverage gap,” Becerra said.
The report from HHS found Medicaid expansion is a signifcant factor in states’ disenrollment numbers.
“The 10 states that have not expanded Medicaid — Alabama, Florida, Georgia, Kansas, Mississippi, South Carolina, Tennessee, Texas, Wisconsin and Wyoming — have disenrolled more children and youth than the 40 states and the District of Columbia that have expanded Medicaid combined,” according to the report.
In an interview with WABE, Gov. Brian Kemp said he is not currently considering fully expanding Medicaid under the Affordable Care Act.
He is promoting the state’s more limited recent expansion of Medicaid in the Georgia Pathways to Coverage program, which offers Medicaid coverage to low-income adults who complete work, education, volunteering or other activity requirements.
“In a way that you have work requirements or people are learning job-training skills or going to school or volunteer and to learn soft skills. And we’re pushing forward on that,” he said.
Pathways has had a sluggish rollout, with fewer than 1,400 people signing up in its first three months.
This week, Kemp announced more than $54 million from the state’s remaining American Rescue Plan Act funds for the state Department of Community Health and the Georgia Department of Human Services to support the agencies’ Medicaid and PeachCare for Kids redetermination processing.
The funding would help expand Medicaid unwinding staffing, improve customer service and eligibility screenings, and boost efforts to keep children covered next year.
Officials called it a “Georgia-specific solution to nationwide challenges with staffing and call volumes due to the fast-approaching deadline to complete Medicaid redetermination efforts,” which is set to be complete by June 2024.
The governor’s office announced key priorities for the funding, including dedicating a so-called surge team of caseworkers to focus on Medicaid renewals next year, call center and email support, and outreach to Medicaid redetermination applicants.
The effort also includes 12 months of continuous eligibility for children in 2024.
State officials say anyone who has already been terminated will, “need to respond within the 90-day reconsideration period or reapply.”
A spokesperson for the Department of Community Health says their Medicaid coverage will not be automatically reinstated.
“This $54 million one-time investment of ARPA funds into Georgia’s public benefit enrollment infrastructure comes at a critical time when Georgians are losing access to healthcare coverage. However, this ‘surge’ support is a Band-Aid on a broken system that needs long-term, sustained funding for staff and person-centered technology that connect Georgians to not just Medicaid but also food assistance and other public benefits,” said the Georgia Budget and Policy Institute’s Chan.








